The Secret World of Pelvic Pain

Pelvic pain is often a world of secrets and subtleties. It can be confusing and alarming. Or it can be totally normalized. Pelvic pain can be disregarded by healthcare professionals or minimized by family, friends, and partners.
It is deciding to not go out for a run during your period, because you can’t wear tampons comfortably. or maybe, it is avoiding sexual experiences with your significant other. It is dreading pelvic exams at your annual doctor’s appointment until it has suddenly been 5 years without going in, because you are too anxious to schedule it. Or it is changing the clothes or underwear that you wear to avoid burning, stabbing, or inflamed sensations from the fabric contacting your skin. It is many things to many women, and it is surprisingly common.
Not every women with pelvic pain has issues with all of these activities. But there are common threads among the stories I hear. Pelvic pain is a hyper-vigilance or unexplainable experience of pain, typically in your pelvic floor. This pain affects your ability to perform your daily activities comfortably. But not all pelvic pain is created equal. I want to demystify this a bit for you.
There are three main categories of pelvic pain that are treated in the physical therapy world.
Vulvodynia:
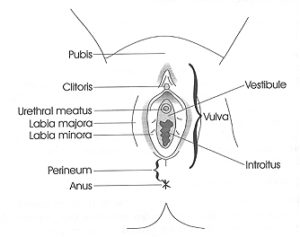
Vulvodynia is a condition where there is pain in any part of the vulva. The vulva contains all of the external female genitalia, including the labia minora, labia majora, clitoris, and mons pubis. This pain could be with sexual contact/stimulation, or with benign contact like from clothing.
Vestibulodynia:
Vestibulodynia is a condition where there is pain in the vestibule. What is the vestibule? Think of the vestibule of a church, or the entryway to the main body of the building. Similarly in the female body, the vestibule is the area that surrounds the openings to the inside, like the vaginal opening, or introitus, and the urethral meatus. The pain with vestibulodynia can feel like dryness, burning, itching, or stabbing pain. It is often associated with redness, swelling, and/or atrophy of the tissues of the vestibule.
Vaginismus:
Vaginismus is pain in or around the vagina, usually with penetration, due to an involuntary contraction of the pelvic floor muscles. This can present as pain with inserting a tampon, pain with sexual contact (called dyspareunia) like inserting a penis, or with a medical pelvic examination like getting a pap smear. Often, women with vaginismus will have pain with all of these. This reflexive contraction of the pelvic floor can be related to physical, emotional, or psychological causes. I wrote a post dedicated solely to the topic of vaginismus over here.
Primary and Secondary
With all of these types of pain, they are further classified as either primary or secondary. Primary pelvic pain means that the pain began as a response to a certain type of stimulus and has continued consistently with that stimulus. Secondary pelvic pain means that the body is now interpreting a stimulus as painful where that stimulus was previously pain-free. Often times, secondary pelvic pain begins after a traumatic or painful experience, like an uncomfortable/unwanted sexual encounter or a particularly difficult pelvic exam that has now conditioned the body to expect pain with those things.
So what can be done?
Counseling/Support:
Pelvic pain is a complicated topic with many facets to it. Pain, in general, can have a huge effect on a person’s life. The effects of pelvic pain are often even more profound on a person’s quality of life and most intimate life experiences. While you seek to address the physical pain, it is also important for many women while healing to seek out psychological and emotional support from a professional. You may also want to consider seeking a counselor that works with couples or families if you know that your pain is having an impact on those closest to you.
Physical Therapy:
If you are intimidated by the idea of going to a pelvic health physical therapist, please read my previous post on what to expect from physical therapy. If you are being treated for pelvic pain, you will likely work on ways to decrease the unhelpful amount of attention that your nervous system is paying to your pelvis. While many therapists take varying approaches, in general, you should not expect to have a therapist put you through a bunch of painful experiences. (And I would argue that the good therapists out there would not do that to you.)
Instead, they will likely begin with pain-free stimuli that you tolerate easily and work from there until you can tolerate common daily stimuli without pain. They may also work with you on “down-training” or decreasing the amount of muscle tension that you have in your pelvic floor muscles while trying to rest. For some women, their pain actually comes from the hyperactivity of the pelvic muscles, especially with vaginismus.
Home Program:
Usually, a counselor and a physical therapist will both give you homework to do on your own, so plan on spending a bit of time each day on that, even if you don’t have an appointment in the clinic that day. It is really important that you make the effort to do these home exercises from your healthcare team, because often times, the work done in the clinic with you isn’t enough to make lasting changes. You have moved and experienced the world in one way for a very long time, so spending a couple of hours per week doing something new will often not be enough to override what you do the rest of the week.
So trust me. Stay committed to the process. Speak up if you don’t understand why you are doing something. Don’t lose hope! It is always a journey to recover from pain. Because real changes doesn’t happen overnight. (And don’t trust anybody that says it does.) It takes some discipline, but it is a very worthwhile journey to seek out help for whatever type of pelvic pain you are experiencing.