Pregnancy-Related Pelvic Girdle Pain
There are many aches and pains that may surface during pregnancy. And, while fleeting pains can occur as a warning signal from your body that you may be overdoing it, pain that limits your sleep or function is not normal. Let me repeat. It is NOT NORMAL to have pelvic girdle pain or back pain in pregnancy. Often times, healthcare providers are dismissive of this pain and say, “it will resolve after you deliver the baby.” Well that is true about most acute back pain, that 90% of the time it will resolve on its own in 6 weeks to 6 months. But we still typically recommend some sort of intervention, like physical therapy, chiropractics, or medication, for acute back pain in a general population. So why do we condemn pregnant women to pain?
It seems that this attitude is prevalent, because, while it is not normal, it is common. The majority of women will either experience low back pain or pain in the pelvic girdle (or both) during their pregnancy as their weight increases and their movement patterns change. Many studies have demonstrated that about 20% of cases of pregnancy-related pelvic girdle pain will be severe with considerable levels of pain and disability and socio-economic consequences. Wow. That doesn’t sound like a condition that we can just continue to ignore as a healthcare community. I believe that leaving this pain untreated has multiple effects.
It makes women have a bad experience in pregnancy, and consequently have fear about having future children.
It is common for me to hear from women that they had a bad experience of pain in pregnancy and don’t think that they could go through that again. And it is even more intimidating when you already have one or more little ones and imagine being pregnant and having too much back or pelvic girdle pain to be able to pick up or care for your children. I have even had physicians tell their patients that they just shouldn’t pick up their toddlers while pregnant, because they are too heavy. So where does that leave women? Likely, feeling disabled and worried that they won’t be able to do their daily tasks while pregnant. In reality, women can get help from physical therapy to manage this pain and allow them to safely participate in their activities of daily living, barring any medical reason that they are restricted (like pre-eclampsia).
It creates compensatory movement patterns that will affect their recovery from pregnancy.
Although I haven’t seen research directly on this topic, I don’t think that it is a huge leap to this conclusion. When I treat a patient that has had a knee injury for a few months, then it is common that, even after their knee pain has resolved, they continue to limp or have less than ideal movement patterns. Our brains are hardwired to avoid pain, whenever possible. So when a pregnant woman is having pain, she will very likely begin to move to avoid aggravating that pain. While the pain may resolve after delivering the baby, her compensations could remain.
It makes it difficult to exercise regularly in pregnancy, therefore making it more difficult to have a fit pregnancy.
When women are in pain, not only is it difficult to fully engage in exercise, but as I mentioned above, they may receive really conservative instructions from a healthcare provider to just stop lifting or moving if it hurts. This does little to encourage fitness and wellness in pregnancy, and usually ends up discouraging it. There are already many myths out there that it isn’t safe to exercise in pregnancy, and pain can falsely corroborate these by the implication that pain is a sign of the danger of movement. (Ironically, many women will experience pain with prolonged sitting or resting even, so the correlation between exercise and pain is very weak.)
It likely predisposes women to back and pelvic girdle pain after pregnancy.
There is evidence that suggests that some women can persist in having pelvic girdle pain long into postpartum, with this study focusing on up to 11 years later. If not screened for or left untreated, it is more likely that a woman will continue to have pelvic pain after delivery.
So what can be done?
Unfortunately, there are not necessarily simple fixes to pelvic girdle pain, because it is true that the contributing factors like weight gain, a shifting of your center of gravity, and maybe even hormone-related joint laxity will get more severe as the pregnancy progresses. But that doesn’t mean it is an uphill battle, unworthy of a fight. Here are some things to remember when looking to reduce pelvic-girdle pain.
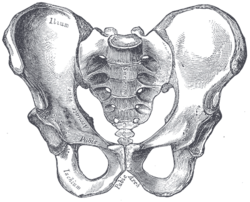
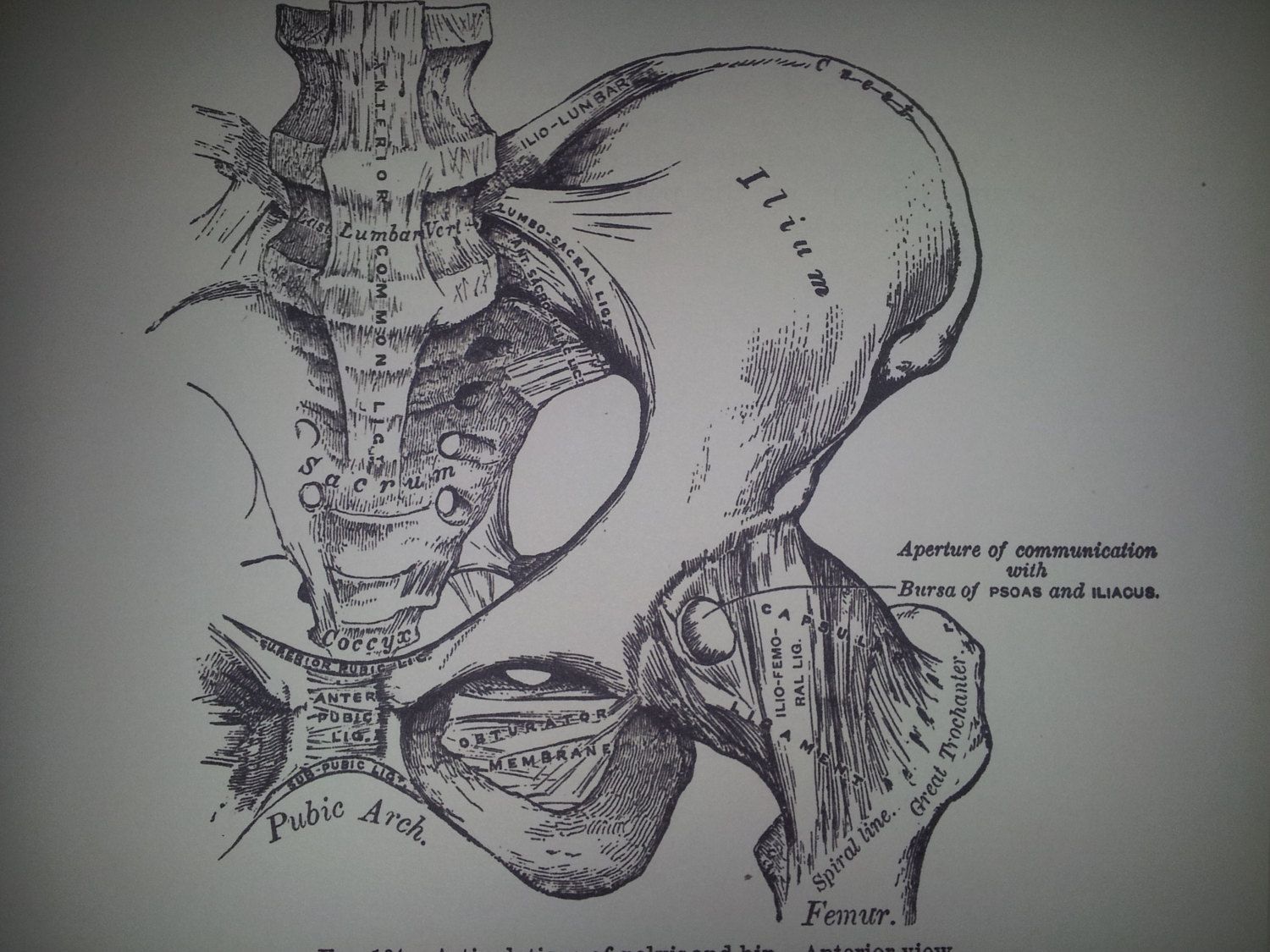
Your pelvis is strong and stable!
Don’t buy into the myths that used to be very popular, even among healthcare professionals, that pelvises are precariously structured and can simply begin to slide around on you in pregnancy. The fact is that pelvises are the main mechanism of transferring force from our legs up to our spine, and they must be able to handle huge loads. So that sensation of “instability” is more likely just a new increase in your nervous system’s awareness. After all, growing a baby inside of that pelvis is a good reason to begin paying extra attention to protecting your body.
Exercise is not dangerous!
While some exercises may aggravate the pain, it is likely not making anything worse or causing any injury. Exercise can actually reduce the symptoms of pelvic girdle pain by causing a desensitization of the nervous system to movement.
If something helps to reduce your pain, use it!
Compression belts and support wear can help some, but not all people. So if you are in the lucky group that feels relief by putting on a compression belt, there is no reason not to. They are safe to use, when worn appropriately down low on the hips around the pelvis (not up around the belly binding your abdomen or limiting your ability to comfortably breathe). Here is my product review on one belt, but there are lots of options out there! The only exception to this principle is if the thing that you are doing to relieve your pain is something your doctor explicitly said don’t do, like sitting in a hot tub or sleeping on your stomach.
When in doubt, seek a professional.
If your pain is persisting, don’t hesitate to continue bringing it up to your doctor or midwife. And if they haven’t referred you on to a physical therapist yet, it is okay to just call a physical therapy clinic directly! In all 50 states in the U.S., PTs have some form of “Direct Access,” meaning you can see them without having to see a doctor and get a referral first.
I hope this helps all of the mamas out there who are already rocking a fit, healthy pregnancy, or those that are doubling down in their commitment to start now!